You are in pain and would like to be referred for an X-ray or MRI to "see what's wrong." This is a perfectly natural request. After all, how can you treat something if you don't know exactly what is broken? This logic seems obvious, but the reality is more nuanced.
Good news: For the vast majority of musculoskeletal pain, a clinical examination with your physical therapist is sufficient to make a diagnosis and establish an effective treatment plan.¹ Imaging would often not change the treatment. What science teaches us about medical imaging:- MRI "abnormalities" are extremely common in people who do not experience any pain.
- What we see in the image does not always correspond to what is causing the pain.
- Imaging can sometimes create more concern than answers.
- In most cases, imaging does not change the recommended treatment plan.
This guide helps you understand when imaging is truly useful. To learn more about the relationship between what we see and what we feel, check out our article on osteoarthritis and pain.
Imaging does not always show what is causing the pain.
When we have an injury or pain, it is in our very nature to want to know the precise structure that is causing us pain.
After all, not knowing what hurts is like not knowing why you have a water leak in the basement: it's anxiety-provoking!
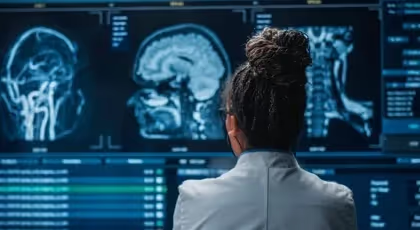
We often place a lot of hope in X-rays, ultrasounds, scans, and magnetic resonance imaging (MRI). We think that by taking a picture of the area where we feel pain, we should be able to find the culprit causing it.
But that is mostly false. In the vast majority of musculoskeletal injuries and pain (pain in the joints, muscles, tendons, nerves, menisci, etc.), a clinical examination (assessment) with a physical therapist is sufficient to make the diagnosis AND determine the best game plan.Moreover, undergoing a medical imaging exam will not change the treatment plan to heal the injury. What does that mean?
Physical assessment
=
Diagnosis Y and treatment plan X
______________
Physical assessment + imaging exam
=
Diagnosis Y again and treatment plan X again
Therefore, a large portion of the imaging exams that are done are completely useless in helping you. It's quite disappointing when we feel like we're getting them precisely to improve our situation!
Even worse, recent studies show that simply receiving a medical imaging result is enough to increase anxiety and negative perception of the injury, in addition to increasing the time it takes to get better. Who would have thought that getting an X-ray for our back pain could be enough to significantly delay our recovery?
So, how can we explain that medical imaging doesn't always help us? There are three fundamental concepts to understand to answer this question:
First, No technology to date allows us to see pain. Pain is an invisible phenomenon that can only be felt and experienced by a person. Pain can be compared to an emotion. No one can "see" sadness. We can see someone who is sad, just as we can see someone who is in pain, but sadness and pain are only experienced by the person who is suffering. Secondly, The things we see in medical imaging (wear and tear, osteoarthritis, tears, etc.) are, in part, normal signs of aging. The older we get, the more small tears we have here and there and wear and tear pretty much everywhere. So it's normal to see this, and it's not necessarily what explains why we're in pain. Thirdly The things we see in imaging are almost as prevalent (and sometimes more so) in people who have no pain. So osteoarthritis in the lower back is just as common in people with back pain as in those without back pain. There must therefore be something else that explains why we feel pain. However, medical imaging should not be thrown away. In cases of trauma or injuries that may require surgery, imaging may be necessary and very useful! Physical therapists are trained to determine whether medical imaging is necessary to determine the best treatment plan for the injury.To summarize, the vast majority of pain and injuries can be treated without the need for medical imaging. The treatment plan will rarely be modified following medical imaging. Pain is never visible on imaging, and its cause is rarely visible. However, when we suspect a fracture or another more serious injury, we will use imaging to rule out serious causes.
To learn more
To learn more For more information on medical imaging, listen to the podcast " Tell me about health " produced by one of our physical therapists, Alexis Gougeon. Episode #27 addresses this topic.Episode #27 of Parle-moi de santé (medical imaging)
You can also find the podcast episode on the following platforms:
Sources:
- Jarvik (2002). Diagnostic evaluation of low back pain with emphasis on imaging. Annals of internal medicine.
- Murphy L (2008). Lifetime risk of symptomatic knee osteoarthritis. Arthritis Care & Research: Official Journal of the American College of Rheumatology.
- Van Tulder (1997). Spinal radiographic findings and nonspecific low back pain: a systematic review of observational studies. Spine.
10 mini-tips to understand your pain
Those who have had the greatest impact on my patients' lives. 1 per day, 2 min.
Our clients' satisfaction is our priority.
At Physioactif, excellence defines our approach. But don't take our word for it, see what our patients are saying.
Discover our physiotherapy clinics
We have multiple locations to better serve you.
Blainville
190 Chem. du Bas-de-Sainte-Thérèse Bureau 110,
Blainville, Quebec
J7B 1A7
Laval
Montreal
St-Eustache
Vaudreuil
21 Cité-des-Jeunes Blvd. Suite 240,
Vaudreuil-Dorion, Quebec
J7V 0N3
Book an appointment now


